The Hunger of Anxiety: Understanding Stress Eating

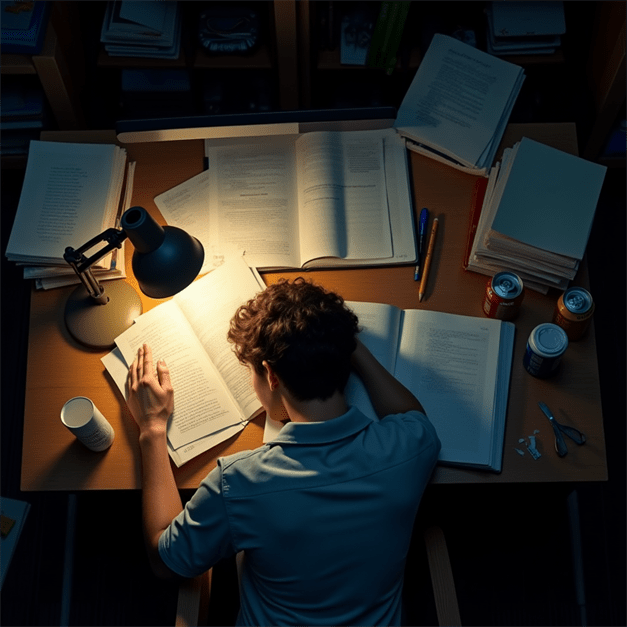
Stress eating has become a common coping mechanism when life gets overwhelming. When deadlines loom, relationships strain, or anxiety peaks, many of us instinctively reach for comfort food to soothe our emotions. This psychological response isn’t simply about hunger—it’s our body’s attempt to regulate stress hormones and find quick relief from mounting pressure.
The cycle of emotional eating often begins with specific triggers that activate our cravings for high-calorie, sugary foods. These comfort foods temporarily boost dopamine and serotonin levels, creating a fleeting sense of pleasure that masks underlying emotional hunger.
Unfortunately, this mindless eating pattern frequently leads to guilt and shame afterward, compounding the very anxiety we were trying to escape. The connection between cortisol—our primary stress hormone—and increased appetite explains why stressful situations so often end with empty ice cream containers and crumpled chip bags.
Breaking free from food coping mechanisms requires developing emotional awareness and alternative self-care strategies. By practicing mindfulness around eating patterns and identifying true hunger signals versus emotional triggers, we can begin to disrupt this self-destructive cycle.
Food journaling can reveal surprising connections between specific stressors and overeating episodes, while learning healthier emotional regulation techniques provides sustainable alternatives to midnight snacking. With patience and practice, the grip of stress eating can loosen, allowing for a more balanced relationship with both food and feelings.
The Connection Between Cortisol and Hunger

Stress triggers a cascade of physiological responses designed to help us survive immediate threats. Unfortunately, our bodies respond to modern psychological stressors—like work deadlines, financial worries, or relationship conflicts—with the same mechanisms evolved for physical dangers.
The Stress Eating Response Pathway
When you experience stress, your body activates the hypothalamic-pituitary-adrenal (HPA) axis:
- Your hypothalamus releases corticotropin-releasing hormone (CRH)
- This triggers your pituitary gland to release adrenocorticotropic hormone (ACTH)
- ACTH stimulates your adrenal glands to produce cortisol
Cortisol, often called the “stress hormone,” plays a crucial role in hunger regulation.
How Cortisol Drives Hunger
Elevated cortisol affects hunger and food preferences through multiple mechanisms:
- Increases ghrelin production: Cortisol stimulates the release of ghrelin, the “hunger hormone,” which signals your brain that it’s time to eat
- Alters insulin sensitivity: Chronic cortisol elevation can reduce insulin sensitivity, leading to blood sugar fluctuations that trigger hunger
- Drives preference for comfort foods: Cortisol specifically enhances cravings for high-calorie, high-carbohydrate “comfort foods”
- Reduces activity in the prefrontal cortex: This brain region responsible for self-control becomes less active under stress, making it harder to resist cravings
The Vicious Cycle
What makes stress-induced hunger particularly challenging is its self-reinforcing nature:
- Stress increases cortisol
- Cortisol triggers hunger and cravings
- Consuming “comfort foods” temporarily reduces stress by activating reward pathways
- This creates a learned association between stress relief and eating
- The cycle continues with each new stressor
Over time, this pattern can become an automatic response, leading to stress eating as a habitual coping mechanism rather than a response to physical hunger.
Different Stress Timing, Different Effects
The timing and duration of stress also influence hunger responses:
- Acute, immediate stress: Often temporarily suppresses appetite as blood flows away from digestive organs toward muscles in preparation for “fight or flight”
- Chronic, ongoing stress: Leads to persistently elevated cortisol and increased appetite, particularly for high-calorie foods
- Post-stress recovery: After acute stress passes, cortisol often remains elevated, triggering heightened hunger during the “recovery” phase
Understanding which type of stress response you’re experiencing can help you recognize and manage stress-induced hunger more effectively.
How Stress Eating Sabotages Weight Loss
Stress eating presents multiple challenges for weight management, extending beyond simply consuming extra calories.
Metabolic Disruption
Chronic stress creates physiological conditions that promote weight gain:
- Increased abdominal fat storage: Cortisol specifically encourages fat deposition in the abdominal area, which is associated with greater health risks
- Slowed metabolism: Prolonged stress can reduce basal metabolic rate, meaning you burn fewer calories at rest
- Disrupted sleep: Stress often impairs sleep quality, which further disrupts hunger hormones and metabolism
- Insulin resistance: Chronic stress can reduce insulin sensitivity, making it harder for your body to process carbohydrates efficiently
Poor Food Choices
Stress doesn’t just make you hungrier—it specifically drives cravings for problematic foods:
- High-calorie preference: Stress increases desire for energy-dense foods high in sugar and fat
- Reward-seeking behavior: The brain seeks rapid dopamine release from highly palatable foods
- Diminished satiety signals: Stress can override normal fullness cues, leading to overeating
- Reduced taste perception: Stress can blunt taste sensitivity, potentially leading to eating more to achieve satisfaction
Behavioral Patterns
Beyond physiological effects, stress creates behavioral patterns that undermine weight management:
- Mindless eating: Stress reduces present-moment awareness, leading to unconscious consumption
- Emotional avoidance: Using food to escape uncomfortable emotions prevents developing healthier coping mechanisms
- All-or-nothing thinking: Stress can trigger perfectionistic thinking where one “bad” choice leads to giving up entirely
- Disrupted routines: Stress often disrupts healthy meal planning and preparation, increasing reliance on convenient but less healthy options
Hormonal Imbalance
Chronic stress creates a hormonal environment conducive to weight gain and resistant to weight loss:
- Leptin resistance: Stress can reduce sensitivity to leptin, the hormone that signals fullness
- Increased neuropeptide Y: This molecule stimulates appetite, particularly for carbohydrates
- Disrupted ghrelin cycles: Irregular ghrelin production leads to hunger signals at inappropriate times
- Reduced production of DHEA: This hormone, which typically counterbalances cortisol’s effects, declines under chronic stress
Ways to Manage Stress Without Food

Breaking the connection between stress and eating requires developing alternative coping strategies. These approaches help manage stress without turning to food:
Physical Release Techniques
Physical activity provides powerful stress relief while supporting weight management:
- Brief intense exercise: Even 10 minutes of high-intensity movement can reduce cortisol and improve mood
- Rhythmic activities: Walking, running, swimming, or cycling create a meditative effect while burning stress hormones
- Tension release methods: Progressive muscle relaxation, stretching, or yoga directly counteract the physical tension caused by stress
- Play and movement: Dancing, recreational sports, or playful activities provide stress relief while shifting focus away from food
The key is finding enjoyable movement that feels like self-care rather than punishment.
Psychological Approaches
Mental techniques can interrupt the stress-hunger connection:
- Mindfulness practices: Regular meditation, even just 5-10 minutes daily, reduces stress reactivity and builds awareness of emotional eating triggers
- “Urge surfing”: Observing cravings with curiosity rather than immediately acting on them
- Cognitive reframing: Identifying and challenging stress-promoting thought patterns
- Guided imagery: Using visualization to mentally rehearse calm responses to stressors
- Deep breathing: Activating the parasympathetic nervous system through slow, diaphragmatic breathing
These practices build the mental space between feeling stressed and automatically reaching for food.
Social Strategies
Human connection provides powerful stress relief:
- Verbalization: Simply describing feelings to a supportive person reduces their intensity
- Scheduled connection: Regular social time with positive people provides preventative stress management
- Support groups: Sharing experiences with others facing similar challenges provides perspective and ideas
- Professional help: A therapist or counselor can provide personalized strategies for breaking stress-eating patterns
- Stress-free socializing: Creating social gatherings not centered around food
Sensory Alternatives
Engaging non-food sensory experiences can satisfy the need for comfort:
- Aromatherapy: Scents like lavender, rose, or sandalwood can reduce stress hormones
- Warm beverages: Herbal tea, bone broth, or warm water with lemon provide comfort without excess calories
- Tactile comfort: Warm baths, soft blankets, or weighted blankets provide physical soothing
- Sound therapy: Calming music, nature sounds, or guided relaxations engage the auditory system
- Visual relaxation: Spending time in nature or looking at calming images activates the parasympathetic nervous system
Best Stress-Reducing Activities
While any positive coping strategy is valuable, research suggests these specific activities offer particularly powerful stress reduction benefits:
Exercise: The Gold Standard
Physical activity stands as the most research-supported stress management technique:
- 30-minute daily walks: Reduced cortisol levels for up to 24 hours
- High-intensity interval training (HIIT): Shown to improve stress resilience when done 2-3 times weekly
- Strength training: Building muscle improves stress hormone regulation
- Mind-body exercise: Yoga, tai chi, and qigong combine movement with breathwork for enhanced stress relief
Research suggests that consistently active people show smaller cortisol spikes when facing stressors compared to sedentary individuals.
Mindfulness Meditation
Regular meditation practice creates measurable changes in stress response:
- Basic mindfulness practice: 10-20 minutes daily of focused attention meditation
- Body scan meditation: Systematically relaxing each body part while bringing awareness to physical sensations
- Loving-kindness meditation: Developing compassion for self and others counteracts stress-promoting thought patterns
- Mindful eating practices: Bringing full awareness to meals helps distinguish emotional from physical hunger
Studies show just 8 weeks of regular meditation practice can reduce cortisol levels by 15%.
Nature Immersion
Time in natural settings offers unique stress-reduction benefits:
- Forest bathing: The Japanese practice of shinrin-yoku (walking slowly through forests) reduces cortisol by up to 16%
- Gardening: Working with soil exposes beneficial microorganisms that may improve mood
- Blue spaces: Time near water bodies shows particularly strong stress-reduction effects
- Green exercise: Physical activity in natural settings amplifies both the stress-reduction and exercise benefits
Research suggests just 20 minutes in a natural setting significantly lowers cortisol levels.
Creative Expression
Artistic activities provide powerful stress relief:
- Journaling: Expressive writing about emotions reduces stress hormones
- Art therapy: Creating visual art reduces cortisol regardless of artistic skill
- Music engagement: Both playing and listening to music can lower stress markers
- Dance: Combining movement, music, and self-expression provides multi-channel stress relief
These activities engage different brain regions than those activated by stress, creating beneficial neural shifts.
Social Connection
Quality social interaction provides a powerful buffer against stress effects:
- Deep conversations: Meaningful discussions with trusted others reduces stress hormones
- Physical touch: Hugs, massage, and physical affection release oxytocin, which counteracts cortisol
- Laughter: Shared humor and laughter reduce stress hormones for up to 24 hours
- Helping others: Volunteer activities shift focus outward and promote purpose
Research shows strong social connections may be the single most significant factor in stress resilience over the lifespan.
Supplements & Lifestyle Changes to Lower Cortisol

Beyond behavioral strategies, certain supplements and lifestyle adjustments can help moderate cortisol levels and reduce stress-induced hunger.
Evidence-Based Supplements
Some natural supplements show promise for stress and cortisol management:
- Ashwagandha: This adaptogenic herb has been shown to reduce cortisol levels by 23-28% in clinical studies
- Phosphatidylserine: May blunt cortisol response to acute stressors
- Omega-3 fatty acids: High-dose EPA/DHA supplementation can reduce cortisol reactivity
- L-theanine: The amino acid found in green tea promotes relaxation without sedation
- Magnesium: Deficiency is linked to increased stress sensitivity and cortisol production
Always consult healthcare providers before starting supplements, especially if taking medications.
Nutritional Approaches
Dietary patterns significantly influence stress hormone regulation:
- Blood sugar stabilization: Regular, balanced meals containing protein and healthy fat prevent cortisol spikes
- Anti-inflammatory foods: Chronic inflammation increases cortisol; foods rich in omega-3s, antioxidants, and polyphenols can help
- Gut health support: The gut-brain axis influences stress response; probiotic-rich foods may help regulate cortisol
- Hydration: Even mild dehydration increases cortisol; aim for 2-3 liters of water daily
- Green tea: Contains both L-theanine and antioxidants that may moderate cortisol
Sleep Optimization
Sleep quality directly impacts cortisol regulation:
- Consistent schedule: Maintaining regular sleep/wake times helps normalize cortisol rhythms
- Morning sunlight: Early light exposure helps regulate the cortisol awakening response
- Evening wind-down: Reducing blue light and stimulation before bed allows proper cortisol decline
- Sleep environment: Cool, dark, quiet sleeping conditions optimize hormonal cycling
- Addressing sleep disorders: Untreated conditions like sleep apnea significantly elevate cortisol
Research suggests even one night of poor sleep can increase cortisol by 45% the following day.
Time Management Strategies
How you structure your day can significantly impact stress levels:
- Time boundaries: Clear work/life separation reduces chronic stress activation
- Priority setting: Distinguishing between urgent and important tasks prevents overwhelm
- Monotasking: Focusing on one activity at a time reduces cognitive load and stress
- Strategic breaks: Short pauses throughout the day prevent stress accumulation
- Saying no: Declining non-essential commitments preserves energy for priorities
Digital Detox Periods
Constant connectivity creates chronic low-level stress:
- Notification management: Limiting alerts reduces stress-inducing interruptions
- Social media boundaries: Scheduled usage times prevent comparison-based stress
- News consumption limits: Controlled exposure to potentially triggering content
- Tech-free zones: Designating spaces (like bedrooms) as device-free areas
- Digital sabbaticals: Regular periods (even hours) completely disconnected from devices
Studies show even brief breaks from digital devices can reduce cortisol levels and stress perception.
Breaking Free From Stress Eating

The connection between stress and hunger is not just psychological—it’s a complex physiological relationship driven by hormones like cortisol that evolved to help us survive threats. In our modern environment, this same system can drive problematic eating patterns that undermine health and weight management.
Understanding the mechanisms behind stress-induced hunger enables you to develop targeted strategies to break this cycle. Physical activity, mindfulness practices, social connection, and physiological approaches to cortisol reduction all offer multiple pathways to manage stress without turning to food.
Remember that stress eating is not a matter of willpower but a natural biological response. Approaching emotional eating with self-compassion while systematically building alternative coping mechanisms creates sustainable change. As you develop a diverse toolkit of non-food stress management techniques, you’ll not only support weight management goals but also build resilience against midnight snacking and comfort cravings that enhances overall wellbeing.